environmental SCIENTIST | A Planetary Prescription | December 2024
Dom Higgins examines the growth of nature prescribing and the benefits to health and society.
Nature transforms people’s lives. Evidence shows that a thriving, wildlife-rich environment benefits both physical and mental health and that people with better access to nature are more active, more mentally resilient and have better all-round health.1
Health and nature: yesterday and today
The nature and health conversation has been around since at least the late nineties – from the development of green gyms at The British Trust for Conservation Volunteers (now The Conservation Volunteers, or TCV) – one of the original ‘green prescriptions’ – to today and the cross-government green social prescribing demonstration programme.2 Most noticeable over the years is that the question has changed from ‘Where is the evidence?’ to ‘How strong is the evidence?’ That is progress.
As far back as 1948, the World Health Organization defined being healthy as a ‘state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity’.3 Will a conventional medical approach achieve this? No. Should it step in when we are ill and need medicine and expert care? Absolutely.
Back to the present day, and the Government has issued a rallying cry to fix the National Health Service (NHS), asking organisations and the public about how they would go about it.4,5 Importantly, the consultation is seeking views on three key shifts as the Government builds the next 10-year health plan for England. Two of these are a significant opportunity for the natural environment sector:
- Spotting illnesses earlier and tackling the causes of ill health; and
- Moving care from hospitals to communities.
Shifting the focus from treating to preventing illness, stopping health problems from developing in the first place, makes sense whichever way you look at it. Prevention, whenever possible, is better for people, the economy and the NHS – and nature has a fundamental role to play. The shift towards community-based health and care is an equally important element: a recognition that a social approach to health and well-being is part and parcel of a sustainable NHS and an essential part of making it fit for the future.

Credit: © Gail Johnson | Adobe Stock
Preventing illness
The NHS cannot cope with the ever-increasing demands placed on it, especially in the winter months. Community-based models of health and well-being, such as social prescribing, are an essential part of a 21st-century health service. Activities that get people together and support them with a wide range of needs, from debt advice to taking up a new interest or hobby, can help ease the pressure on the health system and relieve the burden on mainstream services. With the right policies and investment in prevention, this cycle can be broken.
Local Wildlife Trusts have been partnering up with the NHS for some time, most recently on the Government’s green social prescribing programme. Green prescribing is an evidence-based pillar of social prescribing, which harnesses the power of nature to improve people’s physical and mental health. It involves doctors, health care providers and community groups ‘prescribing’ nature-based programmes to help people overcome preventable health problems. This includes helping those struggling with mental and physical health as well as addressing challenges such as loneliness, physical inactivity and a lack of contact with nature.

Credit: © pongmoji | Adobe Stock
How does green prescribing work?
Social prescribing link workers (and other trusted professionals in allied roles) connect people to community groups and agencies for practical and emotional support, based on a ‘what matters to you’ conversation – rather than a ‘what’s the matter with you?’ one. The original referral can come from a GP clicking a button or from a local community organisation that helps people through a range of non-medical issues that can lead to illness.
The Wildlife Trusts delivers a range of projects and programmes that do this. One example is giving people the opportunity to join one of its regular conservation volunteering groups, which carry out a wide range of tasks – from tree planting and path maintenance to supported smaller-group therapeutic activities, such as food growing, nature walks or crafting. These activities offer participants a wide range of health, well-being and social benefits, particularly those with restricted mobility, older people, carers and those who are economically inactive. It is not unusual for people to come away with new skills and qualifications or with the confidence to progress to more learning or to a job.
A major evaluation of the pilot programme has been published.6 Seven green prescribing pilots began in 2020 – each with involvement from local Wildlife Trusts. Over 8,000 people participated, with 57 per cent coming from the most economically under-served places. This is important because access to high-quality natural places is not equal. Too many people in the UK live in polluted, nature-deprived neighbourhoods:
- One-third of the population does not have nature-friendly places near home. That is nearly 9.5 million households in England;
- 6.7 million children live in areas of the UK where the air is unsafe to breathe – beyond legal limits – leading to 36,000 child deaths every year;7
- People from Black and ethnic minority groups are twice as likely to live in a nature-poor neighbourhoods;8 and
- Access to safe natural spaces for play is unequal, with children in affluent areas being nine times more likely to have access to green places.9

Credit: © Helen Filatova | Adobe Stock
Why does this matter? In 2008, a team at Glasgow University published a study in the Lancet showing the impact of a lack of green space access on health inequalities.10 The study found that the more well-off you are, the greener the neighbourhood where you live is and the less illness you have. Those who were less well-off experienced more illness; however, their health improved with increased exposure to nature where they lived. The poorest in income terms suffered the worst health of all but, critically, the greatest benefit from living somewhere green.
The cross-government demonstration programme also had strong outreach in terms of ethnic diversity, with 21 per cent of people coming from ethnic minority communities. The fact that link workers were able to reach those in areas of high socio-economic deprivation was an important result.6 The Defra report has some eye-catching findings:
- There were big reductions in anxiety and depression symptoms and significant improvements across well-being measures, with big increases in happiness and life satisfaction alongside an increase in people’s feeling that ‘life is worthwhile’.6
- In financial terms, there was a return on investment of £2.42 per £1 invested by HM Treasury: social prescribing generates an economic return. It also compares well with other NHS interventions when looking through a cost-effective lens.
And it seems that HM Treasury is also convinced by this Government-commissioned report, as it has already invested a further £2.3 million in the pilot programme, taking it to March 2025.
The Wildlife Trusts’ 2023 report A Natural Health Service: Improving Lives and Saving Money proves that investing in green prescribing – providing nature-based activities as a health-improvement strategy – is not just the right thing to do for individuals but is also financially prudent for both the public and private sectors.11 Governments, local authorities and businesses all need to get behind a new wave of community-based health programmes and green prescribing is a good place to start.

The economic analysis for the report was carried out by health economists at Ricardo Energy and Environment and the Institute for Occupational Medicine. They analysed five Wildlife Trusts programmes that deliver health-focused nature-based activities. The findings provide compelling evidence that getting involved in nature projects effectively improves people’s health and happiness, which in turn reduces the strain on health care providers – saving the NHS both time and money. The findings suggest that if 1.2 million people took up these kinds of programmes, the NHS could save £100 million a year. By improving individual health and addressing the root causes of health issues, green prescribing leads to an overall decrease in health care needs and associated costs.
The added benefits of the activities offered by organisations like The Wildlife Trusts, Thrive and TCV is that they are relatively inexpensive, easy to replicate and widely accessible. The activities and courses that The Wildlife Trusts run, for instance, are as varied as the people joining them – ranging from gardening to woodwork to wildlife conservation, although can also be as simple as meeting up with others to enjoy a walk in the park.
Wider societal benefits
It is not just individuals that benefit from doing these kinds of things – the knock-on effects help our entire society. For example, Gwent Wildlife Trust’s Wild Health programme was one studied in the report. Participants get to try outdoor activities like coppicing, hedge laying and tree planting. Some become motivated by the work and go on to seek jobs or further opportunities in related areas. This ripple effect positively impacts local economies while improving community spaces. It is a win–win–win story for health, community and business.
Beyond that, it is a huge boost for nature. We need to create wilder and healthier natural places and we need an army of people with skills, knowledge and passion to do the work. Nature’s recovery will not happen overnight, but empowering people to take charge of projects in their communities or to embark on nature-based careers will speed things up at a time when nature needs us most.
There are plenty of commentators talking about the long-term survival of the NHS. Nature can provide some of the answers to these challenges by shouldering the burden on mainstream services. To have the biggest impact, we need to integrate these kinds of programmes into health and social care services across the country. We know green prescribing works, and The Wildlife Trusts report underlines how it makes economic, social and environmental sense to scale up programmes now, not decades into the future. Of course, that requires initial investment, but the returns in terms of social and health benefits are far greater – making green prescribing excellent value for money.
Many illnesses and ailments are preventable – for example, social isolation and loneliness can lead to depression, while physical inactivity can lead to cardiovascular conditions. Green prescribing can help avoid these and stop other health conditions worsening; it can also help people to stay well while they wait for an operation. To put this into context, in May 2023, around 7.3 million people were waiting for an operation – a record high; that is predicted to rise to 10 million, meaning that one in five people could be on a waiting list.12
What is more, the public is crying out for greener, healthier and more natural neighbourhoods. And it is a rather sad indictment of our society that nearly 10 million people in England live in the 1,108 neighbourhoods that are the most deprived of green space.13 Nature is becoming commoditised and a preserve of those who can afford it.
This is not good enough – but it is avoidable. The UK Government has committed to protecting 30 per cent of land for nature by 2030. If this target were achieved in every town and city across the country, far more people would benefit from a wilder, restored natural world, in addition to the health boost for those that live and work near them.
How can this be achieved?
People need to be at the heart of nature’s recovery, and this can happen by working together. An example of this is the Nextdoor Nature project from The Wildlife Trusts. The concept is simple: bring communities together to help nature flourish where they live and work.
Wildlife Trusts across the UK regularly go out into their local areas, knocking on doors and striking up conversations, asking people what they like and what they want to change about their neighbourhoods. From there, skilled staff support those that want to make a change but may not know how. They help them self-organise – sometimes by forming official community groups, other times by coming together around campaigns or local neighbourhood greening projects. Thousands of groups across the UK have been supported by Nextdoor Nature to date, and hundreds more are continuing the work shoulder to shoulder with Wildlife Trusts across the country (see Figure 1):
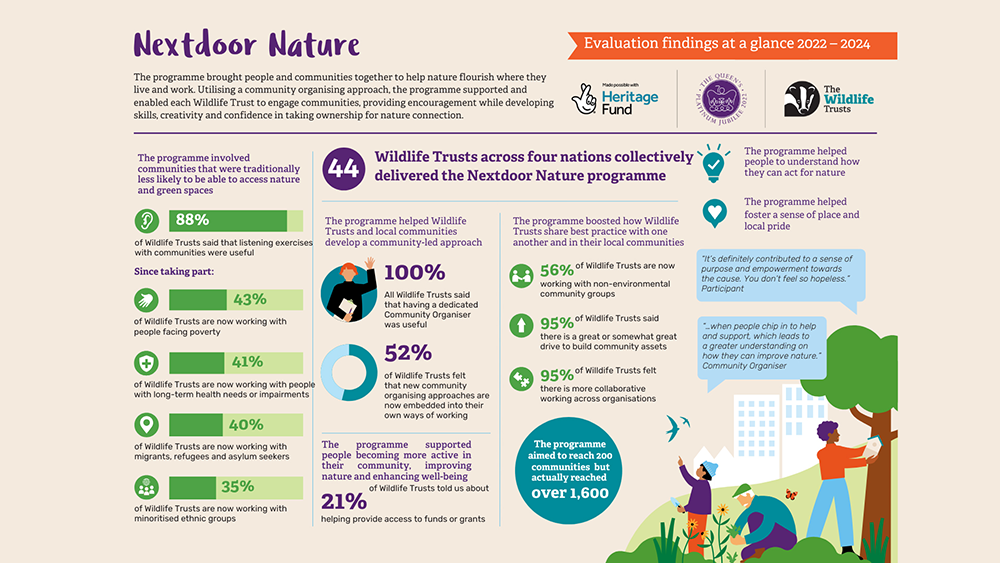 |
| Figure 1. Nextdoor Nature Infographic from the Wildlife Trusts (Source: The Wildlife Trusts) |
Why does all this matter? The more time people spend outside enjoying and learning about nature, the more likely they are to help protect and restore it. We must also provide opportunities for people to spend quality time doing positive things in nature, improving their health, learning new skills, meeting others and fostering deeper connections with the natural world. Approaches through Nextdoor Nature and green prescribing do all these things and more.
We know that nature is an essential part of a community-rooted approach to health and social care: a Natural Health Service to run alongside the National Health Service. But we are not maximising that potential. Green prescribing works, and the more we can develop these kinds of programmes, the greater the benefit to society. The impact it has on societal health is enormous and investing in this work is clearly worth every penny.
Dom Higgins is Head of Health and Education at The Royal Society of Wildlife Trusts where he leads on policy and campaigning. Prior to joining The Wildlife Trusts, he was Director of External Affairs at TCV where he led on the development of a strategic unit to grow the impact of green gyms (one of the original green prescriptions). Previous roles include working for the Department for Education and Skills on its youth and citizenship programmes. Dom chairs Wildlife and Countryside Link’s Nature and Wellbeing Strategy Group and is a member of the Green Social Prescribing Programme board and of the Health Foundation’s strategic advisory board for its Health Equals campaign. He also coaches rugby league and plays in brass bands when time allows!
References
- Department for Environment, Food & Rural Affairs, European Centre for Environment & Human Health, and University of Exeter Medical School (2017) Evidence Statement on the Links between Natural Environments and Human Health. https://beyondgreenspace.net/wp-content/uploads/2017/03/evidence-statement-on-the-links-between-natural-environments-and-human-health1.pdf (Accessed: 28 November 2024).
- NHS England (no date) Green social prescribing. https://www.england.nhs.uk/personalisedcare/social-prescribing/green-social-prescribing/ (Accessed: 28 November 2024).
- World Health Organization (no date) Constitution. https://www.who.int/about/governance/constitution (Accessed: 28 November 2024).
- Department of Health and Social Care (2024) Government issues rallying cry to the nation to help fix NHS. https://www.gov.uk/government/news/government-issues-rallying-cry-to-the-nation-to-help-fix-nhs (Accessed 28 November 2024).
- Change NHS (no date) Home page. https://change.nhs.uk/en-GB/ (Accessed 28 November 2024).
- Department for Environment, Food & Rural Affairs (no date) Preventing and tackling mental ill health through green social prescribing project evaluation – BE0191. https://randd.defra.gov.uk/ProjectDetails?ProjectId=20772 (Accessed: 28 November 2024).
- Office for Health Improvement & Disparities (2022) Air pollution: applying All Our Health. https://www.gov.uk/government/publications/air-pollution-applying-all-our-health/air-pollution-applying-all-our-health (Accessed: 28 November 2024).
- Friends of the Earth (no date) Access to green space in England: are you missing out? https://friendsoftheearth.uk/nature/access-green-space-england-are-you-missing-out (Accessed: 28 November 2024).
- Public Health England (2020) Improving Access to Greenspace: A New Review for 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/904439/Improving_access_to_greenspace_2020_review.pdf (Accessed: 28 November 2024).
- Mitchell, R. and Popham, F. (2008) Effect of exposure to natural environment on health inequalities: an observational population study. Lancet, 372, pp. 1655–1660. DOI: 10.1016/S0140-6736(08)61689-X.
- The Wildlife Trusts (2023) A Natural Health Service: Improving Lives and Saving Money. https://www.wildlifetrusts.org/sites/default/files/2023-07/23JUN_Health_Report_Summary_FINAL.pdf (Accessed: 28 November 2024).
- Royal College of Surgeons of England (2023) NHS waiting list at record high of over 7.3 million. https://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/rtt-waiting-times-march-2023/ (Accessed: 28 November 2024).
- Friends of the Earth (2020) England’s Green Space Gap. How to End Green Space Deprivation in England. https://policy.friendsoftheearth.uk/sites/default/files/documents/2020-10/Green_space_gap_full_report_1.pdf (Accessed: 10 December 2024).
Header image © Rawpixel.com | Adobe Stock




